|
|
 |
|
[DoctorOrFirstname] [Lastname],
|
|
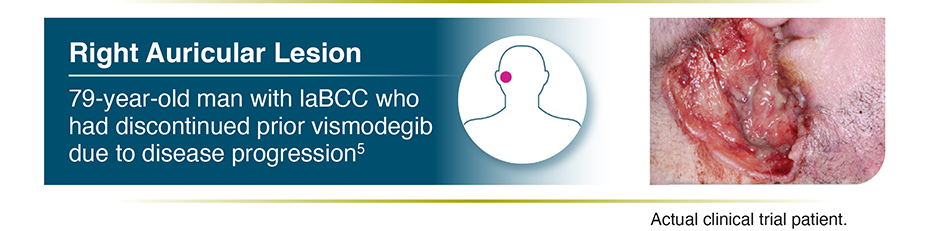
How would you treat the following
patient with locally advanced BCC?
|
|
LIBTAYO is the FIRST AND ONLY treatment indicated for patients with locally advanced basal cell carcinoma (laBCC) previously treated with a hedgehog pathway inhibitor (HHI) or for whom an HHI is not appropriate.1
|
|
|
While most instances of early-stage BCC are curable with surgery and/or radiation,
many patients with advanced disease have a poor prognosis.2-4
|
|
The following patient case study of an laBCC
clinical trial patient treated with LIBTAYO
(cemiplimab-rwlc) may be of interest.5
|
 |
|
LIBTAYO is the #1 most-prescribed
immunotherapy by oncologists in laBCC5*
|
|
*Based on IQVIA medical claims data from October 2018 to December 2021. Claims calibrated with actual vials sold.5
|

|
 |
|
BCC=basal cell carcinoma.
|
|
|
|
|
Important Safety Information
Warnings and
Precautions
Severe and Fatal
Immune‑Mediated Adverse Reactions
|
|
Immune‑mediated adverse reactions, which may be severe or fatal, can
occur in any organ system or tissue at any time after starting treatment.
While immune‑mediated adverse reactions usually occur during
treatment, they can also occur after discontinuation. Immune‑mediated
adverse reactions affecting more than one body system can occur
simultaneously. Early identification and management are essential to
ensuring safe use of PD‑1/PD‑L1–blocking antibodies. The
definition of immune‑mediated adverse reactions included the required
use of systemic corticosteroids or other immunosuppressants and the absence
of a clear alternate etiology. Monitor closely for symptoms and signs that
may be clinical manifestations of underlying immune‑mediated adverse
reactions. Evaluate liver enzymes, creatinine, and thyroid function at
baseline and periodically during treatment. In cases of suspected
immune‑mediated adverse reactions, initiate appropriate workup to
exclude alternative etiologies, including infection. Institute medical
management promptly, including specialty consultation as appropriate.
No dose reduction for LIBTAYO is recommended. In general, withhold LIBTAYO
for severe (Grade 3) immune-mediated adverse reactions. Permanently
discontinue LIBTAYO for life-threatening (Grade 4) immune-mediated adverse
reactions, recurrent severe (Grade 3) immune-mediated adverse reactions that
require systemic immunosuppressive treatment, or an inability to reduce
corticosteroid dose to 10 mg or less of prednisone equivalent per day within
12 weeks of initiating steroids.
Withhold or permanently discontinue LIBTAYO depending on
severity. In general, if LIBTAYO requires interruption or discontinuation, administer
systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or equivalent) until
improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate
corticosteroid taper and continue to taper over at least 1 month. Consider
administration of other systemic immunosuppressants in patients whose
immune‑mediated adverse reactions are not controlled with corticosteroids.
Immune‑mediated
pneumonitis: LIBTAYO can cause immune‑mediated pneumonitis. In
patients treated with other PD-1/PD-L1–blocking antibodies, the incidence of
pneumonitis is higher in patients who have received prior thoracic radiation.
Immune‑mediated pneumonitis occurred in 3.2% (26/810) of patients receiving
LIBTAYO, including Grade 4 (0.5%), Grade 3 (0.5%), and Grade 2 (2.1%). Pneumonitis led
to permanent discontinuation in 1.4% of patients and withholding of LIBTAYO in 2.1% of
patients. Systemic corticosteroids were required in all patients with pneumonitis.
Pneumonitis resolved in 58% of the 26 patients. Of the 17 patients in whom LIBTAYO was
withheld, 9 reinitiated after symptom improvement; of these, 3/9 (33%) had recurrence
of pneumonitis. Withhold LIBTAYO for Grade 2, and permanently discontinue for Grade 3
or 4. Resume in patients with complete or partial resolution (Grade 0 to 1) after
corticosteroid taper. Permanently discontinue if no complete or partial resolution
within 12 weeks of initiating steroids or inability to reduce prednisone to less than
10 mg per day (or equivalent) within 12 weeks of initiating steroids.
Immune‑mediated
colitis: LIBTAYO can cause immune‑mediated colitis. The primary
component of immune‑mediated colitis was diarrhea. Cytomegalovirus (CMV)
infection/reactivation has been reported in patients with corticosteroid-refractory
immune‑mediated colitis treated with PD-1/PD-L1–blocking antibodies. In
cases of corticosteroid-refractory immune‑mediated colitis, consider repeating
infectious workup to exclude alternative etiologies. Immune‑mediated colitis
occurred in 2.2% (18/810) of patients receiving LIBTAYO, including Grade 3 (0.9%) and
Grade 2 (1.1%). Colitis led to permanent discontinuation in 0.4% of patients and
withholding of LIBTAYO in 1.5% of patients. Systemic corticosteroids were required in
all patients with colitis. Colitis resolved in 39% of the 18 patients. Of the 12
patients in whom LIBTAYO was withheld, 4 reinitiated LIBTAYO after symptom
improvement; of these, 3/4 (75%) had recurrence. Withhold LIBTAYO for Grade 2 or 3,
and permanently discontinue for Grade 4. Resume in patients with complete or partial
resolution (Grade 0 to 1) after corticosteroid taper. Permanently discontinue if no
complete or partial resolution within 12 weeks of initiating steroids or inability to
reduce prednisone to less than 10 mg per day (or equivalent) within 12 weeks of
initiating steroids.
Immune‑mediated
hepatitis: LIBTAYO can cause immune‑mediated hepatitis.
Immune‑mediated hepatitis occurred in 2% (16/810) of patients receiving LIBTAYO,
including fatal (0.1%), Grade 4 (0.1%), Grade 3 (1.4%), and Grade 2 (0.2%). Hepatitis
led to permanent discontinuation of LIBTAYO in 1.2% of patients and withholding of
LIBTAYO in 0.5% of patients. Systemic corticosteroids were required in all patients
with hepatitis. Additional immunosuppression with mycophenolate was required in 19%
(3/16) of these patients. Hepatitis resolved in 50% of the 16 patients. Of the 5
patients in whom LIBTAYO was withheld, 3 reinitiated LIBTAYO after symptom
improvement; of these, none had recurrence.
For hepatitis
with no tumor involvement of the liver: Withhold LIBTAYO if AST or ALT
increases to more than 3 and up to 8 times the upper limit of normal (ULN) or if total
bilirubin increases to more than 1.5 and up to 3 times the ULN. Permanently
discontinue LIBTAYO if AST or ALT increases to more than 8 times the ULN or total
bilirubin increases to more than 3 times the ULN.
For hepatitis
with tumor involvement of the liver: Withhold LIBTAYO if baseline AST or ALT
is more than 1 and up to 3 times ULN and increases to more than 5 and up to 10 times
ULN. Also, withhold LIBTAYO if baseline AST or ALT is more than 3 and up to 5 times
ULN and increases to more than 8 and up to 10 times ULN. Permanently discontinue
LIBTAYO if AST or ALT increases to more than 10 times ULN or if total bilirubin
increases to more than 3 times ULN. If AST and ALT are less than or equal to ULN at
baseline, withhold or permanently discontinue LIBTAYO based on recommendations for
hepatitis with no liver involvement.
Resume in patients with complete or partial resolution
(Grade 0 to 1) after corticosteroid taper. Permanently discontinue if no complete or
partial resolution within 12 weeks of initiating steroids or inability to reduce
prednisone to less than 10 mg per day (or equivalent) within 12 weeks of initiating
steroids.
Immune‑mediated
endocrinopathies: For Grade 3 or 4 endocrinopathies, withhold until
clinically stable or permanently discontinue depending on severity.
|
|
• |
Adrenal insufficiency: LIBTAYO can cause
primary or secondary adrenal insufficiency. For Grade 2 or higher adrenal
insufficiency, initiate symptomatic treatment, including hormone replacement as
clinically indicated. Withhold LIBTAYO depending on severity. Adrenal
insufficiency occurred in 0.4% (3/810) of patients receiving LIBTAYO, including
Grade 3 (0.4%). Adrenal insufficiency led to permanent discontinuation of LIBTAYO
in 1 (0.1%) patient. LIBTAYO was not withheld in any patient due to adrenal
insufficiency. Systemic corticosteroids were required in all patients with adrenal
insufficiency; of these, 67% (2/3) remained on systemic corticosteroids. Adrenal
insufficiency had not resolved in any patient at the time of data cutoff
|
|
• |
Hypophysitis: LIBTAYO can cause
immune‑mediated hypophysitis. Hypophysitis can present with acute
symptoms associated with mass effect such as headache, photophobia, or
visual field defects. Hypophysitis can cause hypopituitarism. Initiate
hormone replacement as clinically indicated. Withhold or permanently
discontinue depending on severity. Hypophysitis occurred in 0.4% (3/810) of
patients receiving LIBTAYO, including Grade 3 (0.2%) and Grade 2 (0.1%)
adverse reactions. Hypophysitis led to permanent discontinuation of LIBTAYO
in 1 (0.1%) patient and withholding of LIBTAYO in 1 (0.1%) patient. Systemic
corticosteroids were required in 67% (2/3) of patients with hypophysitis.
Hypophysitis had not resolved in any patient at the time of
data cutoff |
|
|
• |
Thyroid disorders: LIBTAYO can cause
immune‑mediated thyroid disorders. Thyroiditis can present with or without
endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate hormone
replacement or medical management of hyperthyroidism as clinically indicated.
Withhold or permanently discontinue LIBTAYO depending on severity |
|
• |
Thyroiditis: Thyroiditis occurred in 0.6%
(5/810) of patients receiving LIBTAYO, including Grade 2 (0.2%) adverse reactions.
No patient discontinued LIBTAYO due to thyroiditis. Thyroiditis led to withholding
of LIBTAYO in 1 patient. Systemic corticosteroids were not required in any patient
with thyroiditis. Thyroiditis had not resolved in any patient at the time of data
cutoff. Blood thyroid stimulating hormone increased and blood thyroid stimulating
hormone decreased have also been reported |
|
• |
Hyperthyroidism: Hyperthyroidism
occurred in 3.2% (26/810) of patients receiving LIBTAYO, including Grade 2
(0.9%). No patient discontinued treatment and LIBTAYO was withheld in 0.5%
of patients due to hyperthyroidism. Systemic corticosteroids were required
in 3.8% (1/26) of patients. Hyperthyroidism resolved in 50% of 26 patients.
Of the 4 patients in whom LIBTAYO was withheld for hyperthyroidism, 2
patients reinitiated LIBTAYO after symptom improvement; of these, none had
recurrence of hyperthyroidism |
|
|
• |
Hypothyroidism: Hypothyroidism
occurred in 7% (60/810) of patients receiving LIBTAYO, including Grade 2
(6%). Hypothyroidism led to permanent discontinuation of LIBTAYO in 1 (0.1%)
patient. Hypothyroidism led to withholding of LIBTAYO in 1.1% of patients.
Systemic corticosteroids were not required in any patient with
hypothyroidism. Hypothyroidism resolved in 8.3% of the 60 patients. Majority
of the patients with hypothyroidism required long-term thyroid hormone
replacement. Of the 9 patients in whom LIBTAYO was withheld for
hypothyroidism, 1 reinitiated LIBTAYO after symptom improvement; 1 required
ongoing hormone replacement therapy |
|
|
• |
Type 1 diabetes mellitus, which can present with
diabetic ketoacidosis: Monitor for hyperglycemia or other signs and
symptoms of diabetes. Initiate treatment with insulin as clinically indicated.
Withhold LIBTAYO depending on severity. Type 1 diabetes mellitus occurred in 0.1%
(1/810) of patients, including Grade 4 (0.1%). No patient discontinued treatment
due to type 1 diabetes mellitus. Type 1 diabetes mellitus led to withholding of
LIBTAYO in 0.1% of patients |
|
|
Immune‑mediated nephritis with
renal dysfunction: LIBTAYO can cause immune‑mediated nephritis.
Immune‑mediated nephritis occurred in 0.6% (5/810) of patients receiving
LIBTAYO, including fatal (0.1%), Grade 3 (0.1%), and Grade 2 (0.4%). Nephritis led to
permanent discontinuation in 0.1% of patients and withholding of LIBTAYO in 0.4% of
patients. Systemic corticosteroids were required in all patients with nephritis.
Nephritis resolved in 80% of the 5 patients. Of the 3 patients in whom LIBTAYO was
withheld, 2 reinitiated LIBTAYO after symptom improvement; of these, none had
recurrence. Withhold LIBTAYO for Grade 2 or 3 increased blood creatinine, and
permanently discontinue for Grade 4 increased blood creatinine. Resume in patients
with complete or partial resolution (Grade 0 to 1) after corticosteroid taper.
Permanently discontinue if no complete or partial resolution within 12 weeks of
initiating steroids or inability to reduce prednisone to less than 10 mg per day (or
equivalent) within 12 weeks of initiating steroids.
Immune‑mediated
dermatologic adverse reactions: LIBTAYO can cause immune‑mediated
rash or dermatitis. Exfoliative dermatitis, including Stevens-Johnson syndrome (SJS),
toxic epidermal necrolysis (TEN), and drug rash with eosinophilia and systemic
symptoms (DRESS) has occurred with PD-1/PD-L1–blocking antibodies.
Immune‑mediated dermatologic adverse reactions occurred in 1.6% (13/810) of
patients receiving LIBTAYO, including Grade 3 (0.9%) and Grade 2 (0.6%).
Immune‑mediated dermatologic adverse reactions led to permanent discontinuation
in 0.1% of patients and withholding of LIBTAYO in 1.4% of patients. Systemic
corticosteroids were required in all patients with immune‑mediated dermatologic
adverse reactions. Immune‑mediated dermatologic adverse reactions resolved in
69% of the 13 patients. Of the 11 patients in whom LIBTAYO was withheld for
dermatologic adverse reactions, 7 reinitiated LIBTAYO after symptom improvement; of
these, 43% (3/7) had recurrence of the dermatologic adverse reaction. Topical
emollients and/or topical corticosteroids may be adequate to treat mild to moderate
non-exfoliative rashes. Withhold LIBTAYO for suspected SJS, TEN, or DRESS. Permanently
discontinue LIBTAYO for confirmed SJS, TEN, or DRESS. Resume in patients with complete
or partial resolution (Grade 0 to 1) after corticosteroid taper. Permanently
discontinue if no complete or partial resolution within 12 weeks of initiating
steroids or inability to reduce prednisone to less than 10 mg per day (or equivalent)
within 12 weeks of initiating steroids.
Other immune‑mediated
adverse reactions: The following clinically significant
immune‑mediated adverse reactions occurred at an incidence of <1% in 810
patients who received LIBTAYO or were reported with the use of other
PD-1/PD-L1–blocking antibodies. Severe or fatal cases have been reported for
some of these adverse reactions.
|
|
• |
Cardiac/vascular: Myocarditis,
pericarditis, and vasculitis. Permanently discontinue for Grades 2, 3, or 4
myocarditis |
|
• |
Nervous system: Meningitis,
encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia
gravis (including exacerbation), Guillain-Barré syndrome, nerve
paresis, and autoimmune neuropathy. Withhold for Grade 2 neurological
toxicities and permanently discontinue for Grades 3 or 4 neurological
toxicities. Resume in patients with complete or partial resolution (Grade 0
to 1) after corticosteroid taper. Permanently discontinue if no complete or
partial resolution within 12 weeks of initiating steroids or inability to
reduce prednisone to less than 10 mg per day (or equivalent) within 12 weeks
of initiating steroids |
|
|
• |
Ocular: Uveitis, iritis, and other ocular
inflammatory toxicities. Some cases can be associated with retinal detachment.
Various grades of visual impairment to include blindness can occur. If uveitis
occurs in combination with other immune‑mediated adverse reactions, consider
a Vogt-Koyanagi-Harada–like syndrome, as this may require treatment with
systemic steroids to reduce the risk of permanent vision loss |
|
• |
Gastrointestinal: Pancreatitis to include
increases in serum amylase and lipase levels, gastritis, duodenitis, stomatitis
|
|
• |
Musculoskeletal and connective
tissue: Myositis/polymyositis, rhabdomyolysis, and associated
sequelae including renal failure, arthritis, polymyalgia rheumatica |
|
|
• |
Endocrine: Hypoparathyroidism |
|
• |
Other (hematologic/immune): Hemolytic
anemia, aplastic anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis),
sarcoidosis, immune thrombocytopenic purpura, solid organ transplant rejection
|
|
|
Infusion-related
reactions
Severe infusion-related reactions (Grade 3) occurred in
0.1% of patients receiving LIBTAYO as a single agent. Monitor patients for signs and
symptoms of infusion-related reactions. The most common symptoms of infusion-related
reaction were nausea, pyrexia, rash, and dyspnea. Interrupt or slow the rate of
infusion for Grade 1 or 2, and permanently discontinue for Grade 3 or 4.
Complications of allogeneic HSCT
Fatal and other serious complications can occur in patients
who receive allogeneic hematopoietic stem cell transplantation (HSCT) before or after
being treated with a PD-1/PD-L1–blocking antibody. Transplant-related
complications include hyperacute graft-versus-host disease (GVHD), acute GVHD, chronic
GVHD, hepatic veno-occlusive disease (VOD) after reduced intensity conditioning, and
steroid-requiring febrile syndrome (without an identified infectious cause). These
complications may occur despite intervening therapy between PD-1/PD-L1 blockade and
allogeneic HSCT. Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus risks of treatment
with a PD-1/PD-L1–blocking antibody prior to or after an allogeneic HSCT.
Embryo-fetal
toxicity
LIBTAYO can cause fetal harm when administered to a
pregnant woman due to an increased risk of immune‑mediated rejection of the
developing fetus resulting in fetal death. Advise women of the potential risk to a
fetus. Advise females of reproductive potential to use effective contraception during
treatment with LIBTAYO and for at least 4 months after the last dose.
|
|
Adverse Reactions
|
|
• |
In the pooled safety analysis of 810 patients, the most common adverse reactions
(≥15%) with LIBTAYO were musculoskeletal pain, fatigue, rash, and diarrhea
|
|
• |
In the pooled safety analysis of 810 patients, the most common Grade 3-4
laboratory abnormalities (≥2%) with LIBTAYO were lymphopenia, hyponatremia,
hypophosphatemia, increased aspartate aminotransferase, anemia, and
hyperkalemia
|
|
|
|
Use in Specific Populations |
|
• |
Lactation: Because of the potential for
serious adverse reactions in breastfed children, advise women not to breastfeed
during treatment and for at least 4 months after the last dose of LIBTAYO |
|
• |
Females and males of reproductive
potential: Verify pregnancy status in females of reproductive
potential prior to initiating LIBTAYO |
|
|
|
LIB.21.02.0051
|
|
Please click here for full Prescribing
Information.
For more
information, visit LIBTAYOhcp.com
For
prescribers in Colorado, please click here for pricing
information.
References: 1. LIBTAYO (cemiplimab-rwlc) injection full U.S. prescribing information. Regeneron Pharmaceuticals, Inc.
2. Puig S, Berrocal A. Management of high-risk and advanced basal cell carcinoma.Clin Transl Oncol. 2015;17(7):
497-503.
3. Migden MR, Chang ALS, Dirix L, Stratigos AJ, Lear JT. Emerging trends in the treatment of advanced basal
cell carcinoma. Cancer Treat Rev. 2018;64:1-10.
4. Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma:
epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol.
2019;80(2):303-317.
5. Data on file. Regeneron Pharmaceuticals, Inc.
|
|
Let’s connect soon. Click below to be contacted by a Regeneron Oncology
Account Specialist to discuss LIBTAYO® (cemiplimab-rwlc)
|
 |
|
|
|
|
© 2023 Regeneron Pharmaceuticals, Inc.
All rights
reserved.
LIB.22.12.0055 01/23
The message was sent by:
MyDrugRep.com on behalf of Regeneron
Pharmaceuticals, Inc.
MyDrugRep.com/D+R
Lathian • 197 State Route 18
South • South Wing, Suite
3000 • East Brunswick, NJ 08816
This message and any attachments are for the designated
recipient only and may contain privileged, proprietary, or otherwise private
information. If you have received it in error, please notify the sender immediately
and delete the original. Any other use of the email by you is prohibited.
MyDrugRep.com
Privacy Policy
Unsubscribe
from future messages from MyDrugRep.com
|
|
|
|